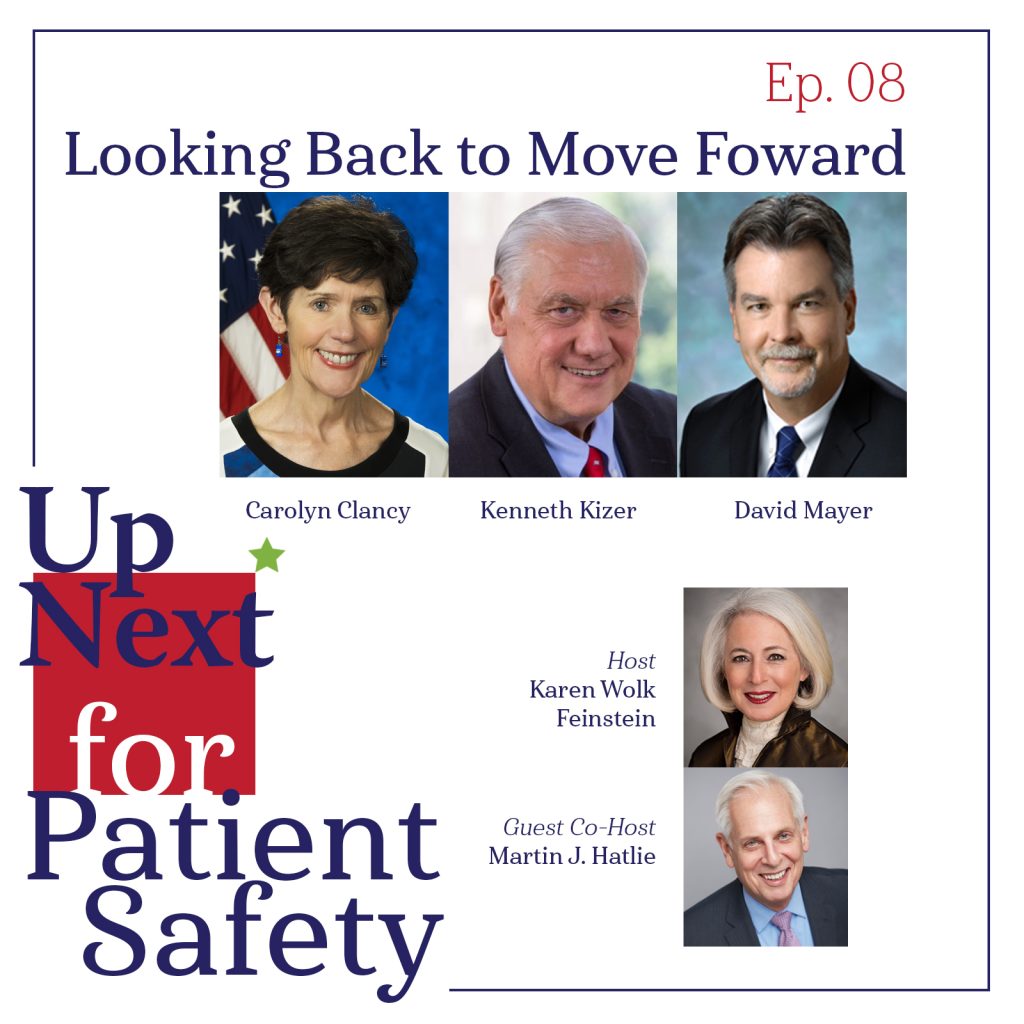
Episode 08: Looking Back to Move Forward
In a special episode to kick off the new year, three renowned leaders in patient safety offer critical insight on where we’ve come from and how to move forward. Join host Karen Wolk Feinstein and special guest co-host Martin Hatlie of Project Patient Care and MedStar Institute for Quality & Safety in a compelling conversation with Dr. Carolyn Clancy of the Veterans Health Administration, Dr. Kenneth Kizer of Atlas Research, and Dr. David Mayer of MedStar Institute for Quality & Safety as they reflect on the origins of the patient safety movement and look toward the future of patient safety in the U.S. They help us understand what the history of efforts to improve patient safety can tell us about what can be done today to eliminate patient harm.
Listen to this episode on: Apple Podcasts | Spotify
Featured Speakers
- Carolyn Clancy, MD, Assistant Under Secretary for Health for Discovery, Education and Affiliate Networks, Veterans Health Administration
- Karen Wolk Feinstein, PhD, President & CEO, Jewish Healthcare Foundation & Pittsburgh Regional Health Initiative
- Martin J. Hatlie, JD, President & CEO, Project Patient Care, and Director, MedStar Institute for Quality and Safety
- Kenneth W. Kizer, MD, MPH, Chief Healthcare Transformation Officer and Senior Executive Vice President, Atlas Research
- David Mayer, MD, Executive Director, MedStar Institute for Quality & Safety, and former Chief Executive Officer, Patient Safety Movement Foundation
Referenced Resources (in order of appearance)
- World Health Organization: Patient Safety (World Health Organization)
- Serious Reportable Events “Never Events” (National Quality Forum)
- A doctor walks to Wrigley Field as part of his 2,600-mile journey to hit every MLB ballpark, raising awareness about preventable deaths in health care settings (Chicago Tribune, 2020)
- To Err is Human: Building a Safer Health System (Institute of Medicine, 1998)
- Five Years After IOM Report on Medical Errors, Nearly Half of All Consumers Worry About the Safety of Their Health Care (Kaiser Family Foundation, 2004)
- National Survey on Consumers’ Experiences With Patient Safety and Quality Information (Kaiser Family Foundation, 2004)
- Remarks by the President on Health Care: The Rose Garden (Clinton Administration, 1999)
- Renaming the Agency for Healthcare Policy and Research (Federal Register)
- Making Health Care Safer: A Critical Analysis of Patient Safety Practices (AHRQ, 2001)
- AHRQ Research Findings & Reports (AHRQ)
- What is Six Sigma? (American Society for Quality)
- What is Lean? (Lean Enterprise Institute)
- Quality Measurement and Quality Improvement (CMS)
- Master of Science in Patient Safety Leadership Program (University of Illinois Chicago)
- The Academy for Emerging Leaders in Patient Safety: The Telluride Experience – About Page
- Up Next for Patient Safety – Episode 07: Anesthesiology’s Answer
- National Surgical Quality Improvement Program (PSNet – AHRQ, 2008)
- Critical Role of the Surgeon-Anesthesiologist Relationship for Patient Safety (ASA, 2018)
- The Origins, Evolution, and Spread of Anesthesia Monitoring Standards: From Boston to Across the World (Anesthesia & Analgesia, 2021)
- Epidemiology of Anesthesia-related Mortality in the United States, 1999-2005 (Anesthesiology, 2009)
- Beyond ‘John of AHRQ’ – John Eisenberg at Penn Medicine, Wharton and LDI: A Profile of One of the True Greats of Health Services Research (University of Pennsylvania: Leonard Davis Institute, 2017)
- Peer Review of a Report on Strategies to Improve Patient Safety (National Academy of Medicine, 2021)
- Strategies to Improve Patient Safety: Draft Report to Congress for Public Comment and Review by the National Academy of Medicine (AHRQ, 2021)
- John M. Eisenberg Patient Safety and Quality Awards (The Joint Commission)
- Paul H. O’Neill, Sr. In Memoriam (Value Capture LLC, 2020)
- The mental health of healthcare workers in the COVID-19 pandemic: A systematic review (Journal of Diabetes & Metabolic Disorders, 2020)
- When Doctors Struggle With Suicide, Their Profession Often Fails Them (NPR, 2018)
- ‘Are You Going to Keep Me Safe?’ Hospital Workers Sound Alarm on Rising Violence (Kaiser Health News, 2021)
- Get Us PPE – Mission and Values
- Announcement of the National Patient Safety Partnership (Veterans Administration, 1997)
- Patient Safety Moonshot (Patient Safety Movement Foundation)
- Wyden, Casey Unveil Comprehensive Bill to Improve Nursing Homes for Residents and Workers (U.S. Senate Committee on Finance, 2021)
- State-Based Reporting in Healthcare (National Quality Forum)
- Adverse Events Reporting System (Minnesota Department of Health)
- Aviation Safety Information Analysis & Sharing Overview (ASIAS)
- Global Patient Safety Action Plan 2021-2030 (WHO, 2021)
- Partnership for Patients (CMS)
- What is the Health Care Payment Learning & Action Network? (HCPLAN)
- An Autonomous Semi-Truck Just Drove Across America to Deliver Butter (Forbes, 2019)
Episode Transcript
[00:00:00] Carolyn Clancy: …Improving patient safety is a team sport, but no specialty or individual group of physicians can do it alone…
[00:00:08] David Mayer: …We know the healthcare system is not safe for those receiving care, but it is also very dangerous for those that are providing care…
[00:00:16] Marty Hatlie: …And when I talked to them, they said, “there’s nobody in charge, we don’t know who’s in charge of patient safety in this country…”
[00:00:22] Ken Kizer: …COVID Pandemic and in all of its ramifications and complexities provides a lot of opportunities to highlight and showcase this issue…
[00:00:35] Karen Wolk Feinstein: Welcome back to Up Next for Patient Safety, where we envision a world where medical errors, adverse events and preventable harms are avoided. And where we examine the most promising paths to prevent these tragedies before they occur. I’m your host, Karen Feinstein, CEO, and president of the Jewish Healthcare Foundation and the Pittsburgh Regional Health Initiative, which is a multi-stakeholder quality collaborative. We’ve been working to reduce medical error for over 20 years, mostly unsuccessfully, but we can’t give up because there’s too much at stake. And that is the loss of approximately 250,000 lives a year and long-term injuries for many more.
Today, I’m joined by a great leader in the patient safety movement and a good friend, Marty Hatlie, who has been working to reduce medical error even longer than we have at the Pittsburgh Regional Health Initiative. Marty will help moderate today’s conversation.
He’s CEO of Project Patient Care, a nonprofit organization that uses the voice of the patient to improve care. It’s mission is to mobilize diverse healthcare stakeholders in metropolitan Chicago to provide the best possible care to every patient, every time by eliminating preventable harm and implementing systemic change to ensure consistent excellence. He also is co-director of the MedStar Institute for Quality and Safety. Marty works internationally with the World Health Organization’s Patient Safety program, and he may be the best networker in the patient safety world today. Marty!
[00:02:09] Marty Hatlie: Thanks, Karen, it’s great to join you today for this conversation. Let me start by thanking you also, and the Jewish Healthcare Foundation and the Pittsburgh Regional Health Initiative for your tireless activity in this field as well. And I want to echo that we can’t just give up on this because the problem is too big, patient safety is fundamental. We all know that and we’re going to have a great program about that today.
And although we haven’t seen the improvement in outcomes we hoped for 20 years ago, when we first embraced this as a big issue, we’ve learned a lot through trial and error over the last 20 years – 20 plus years – and that learning can inform our work going forward. So I remain optimistic that real change is achievable, and we get the opportunity to explore that today with some great panelists.
[00:02:53] Karen Wolk Feinstein: Well, bear with me while I make introductions because we have a special episode today joined by a panel of passionate patient safety advocates. Each has initiated the innovations that advanced patient safety and all have been well-recognized for their achievements. So, let’s reminisce, reflect, and look to the future.
Dr. Carolyn Clancy is the assistant undersecretary for health, for discovery, education, and affiliate networks at the Veteran’s Health Administration. Prior to that, she served as the VHA executive-in-charge. Dr. Clancy also served as the deputy undersecretary for health, for organizational excellence, overseeing VHA’s performance, quality, safety, risk management, systems engineering, auditing oversight, ethics, and accreditation program as well for 10 years as the director of the Agency for Healthcare Research and Quality.
Let me just say from my own personal experience, there’s nothing quote “under” end-quote about Carolyn. In 2015, Dr. Clancy was selected as the outstanding federal executive of the year by disabled American vets. Dr. Clancy’s a general internist and health services researcher. And I’m proud to say, graduate of Boston college and the University of Massachusetts Medical School. She holds an academic appointment at George Washington University School of Medicine and serves as senior associate editor, health services research.
Let’s move now to Dr. Ken Kizer. The chief healthcare transformation officer and senior executive vice president of Atlas Research. He leads Atlas’ efforts to provide clients with pioneering health care solutions and innovations. Dr. Kizer is internationally respected for his many accomplishments in health system transformation, patient safety and quality improvement, and others. He’s best known to me for his acclaimed transformation of the Veteran’s Healthcare System, the nation’s largest in the late 1990s, when serving as the VA’s undersecretary for health. He also is the founder of the National Quality Forum. And he established the concept of never events and safe practices.
Dr. David Mayer is the former CEO of the Patient Safety Movement Foundation and remains a director on the governance board. Dr. Mayer is executive director of the MedStar Institute for Quality and Safety. In this role, he leads specific quality and safety programs in support of discovery, learning, and the application of innovative methods to operational clinical challenges. Prior to his appointment as executive director, he served for over six years as vice-president of quality and safety for MedStar health. He also designs and directs system-wide activity for patient safety and risk reduction. Last year at the height of COVID-19, Dr. Mayer walked over 3000 miles – this is true, we got to meet him along the way – to raise awareness for patient and health worker safety. Dave, I’m sure you have a book and a movie coming from this experience.
I welcome all three panelists. We’re absolutely delighted you’re joining us today and I’m going to turn this over for the first question to Marty.
[00:06:05] Marty Hatlie: Okay, thanks. Karen. I’d like to start with, To Err is Human, the Institute of Medicine’s, groundbreaking call to action on patient safety 20 years ago, more than 20 years ago now, when it was released on November 30th, 1999, it had a huge impact. Polling showed that a week later, more than 50% of Americans were aware of that report. And all of our panelists were already involved and engaged in patient safety that time. So my question really was, did the strength of the reaction surprise to you and what were you doing already when the report came out and how did it shape the work that you did going forward? Carolyn, why don’t we start with you?
[00:06:43] Carolyn Clancy: Sure. Thanks, Marty. So was I surprised a little bit, yes. I think I was surprised by the magnitude of the reaction. On the other hand, when the report came out for the first time ever in the Institute of Medicine’s history, this was announced from a Rose Garden ceremony by President Clinton, which of course does elevate it to a certain place. And I think the number 98,000… up to 98,000 deaths that could have been avoided really got people’s attention. This was not abstract, this was real. And after a while, people got that, you could go into a healthcare setting for one problem and acquire something else that had may or may not have anything to do with why you were initially sought care. So the reaction was quite amazing.
I was in a senior position at AHRQ at that time, which then had a different name and it had a huge impact on what we did going forward. AHRQ became the leading funder for patient safety research. At the time we were going through reauthorization and actually that was part of a name change and it also positioned AHRQ as the lead across the government, making sure that all parts of government were working together on patient safety together. So yes, I would say it had a big impact and very, very importantly, we had a series of hearings where people could give testimony about what they thought were important problems in patient safety. I can’t even tell you, I mean, the phone lines and emails were jammed because so many people wanted to share their thoughts. Providers had to be limited to three minutes and we had to have two overflow sessions to hear from all of them. So a huge impact.
[00:08:30] Marty Hatlie: Carolyn I remember that too. And I remember thinking that it was, it was almost like somebody had acknowledged the secret to something that we knew was happening and maybe we didn’t have the numbers or didn’t – we’re comfortable talking about it – but suddenly here was the report and it wasn’t a secret anymore. And in terms of the research, I also remember when AHRQ did that first sort of survey of what we had evidence for that would improve safety… there were like 26 or 27 things. And when I look back now at what has been produced and accomplished by AHRQ in terms of just adding to the evidence-based and the tools we’ve got, I mean, It’s a prodigious body of work.
Dave, what about you? What were you doing then? And were you surprised when this came up?
[00:09:15] David Mayer: Well, Marty, surprisingly, I was the medical director at Abbott Labs at the time. Here’s a story few people know, I left clinical practice for four years because our hospital leadership refused to address the poor outcomes of one of our surgeons I worked closely with. The physical and emotional toil was beginning to break me and my family noticed it, especially my wife and my children, so they convinced me to resign my position as director of cardiothoracic anesthesia at the time and accept the offer from Abbott. And I will tell you it was the best move I ever made.
I learned things like Six Sigma, Lean, quality improvement, effective teamwork and leadership skills. Skills, no one ever taught me during medical school, residency, or as an attending at the hospital. Well, after the report came out in late 2001, I was recruited back to the medical center because our leadership now understood many of the things I had been warning them and others have been warning them about for years. They recruited me back so I could help lead quality and safety at the university and the medical center. And they all also made me associate dean, academic dean of the medical school there. And I’m proud to say two years after I got there, we had implemented the first four-year longitudinal patient safety and quality care curriculum in a medical school.
So as you know, and you’ve heard me say for many years, I really believe the most effective way to start changing culture is by educating the workers.
[00:10:45] Marty Hatlie: Right. David, you went on to, I think start a master’s program in patient safety too at the University of Illinois. And then subsequently, when I think about your career, it’s been a deep, deep dedication to learning in this space and teaching others.
[00:11:00] David Mayer: So many things go to Carolyn who seeded our first Telluride patient safety round table in Colorado in 2005. And over the course of the last, almost 20 years, we brought over 1400 medical students, residents, and nursing students out to Colorado and Washington and the other parts of the country to put them through four days of workshops on patient safety. That all started with an AHRQ small grant.
[00:11:29] Marty Hatlie: Fantastic. I kind of remember what you were doing at that time, because you were at the VA and you were already a leader in this space before the IOM report came out. But what surprised you about the report and how did it shape the future of your career, Ken?
[00:11:46] Ken Kizer: Yeah, actually, when the report came out, I was three months into trying to establish this new organization known as the National Quality Forum. I am at the VA, although as you say, I’ve been deeply involved in the issues for some years and had actually been on the IOM group that was a predecessor to To Err is Human. So based on that, nothing that was in the report was a surprise, the information and the data was well-known. The reaction was interesting and I think something that is often overlooked that part of the media storm that ensued from when the report was released was because one of the media outlets was going to break the embargo on the report and that kind of catalyzed a media frenzy when the report was actually released on December.
But I think their report was extremely helpful in getting the National Quality Forum going and focusing attention. Indeed, our first projects, which were – as Carolyn mentioned were catalyzed by an event that President Clinton held in the Rose Garden – was to establish these things that ultimately became known as never events and some of the other early work that the NQF did.
[00:13:02] Marty Hatlie: Okay, well, great. Thanks, Ken. And I know, I mean, my memory from that time is that just leaders emerged, and leaders really took this on as a priority. So we’ll come back to that a little bit later with a question, but Karen, I think you’ve got the next question for our team here.
[00:13:20] Karen Wolk Feinstein: Yes, well, in a recent podcast, I interviewed Jeff Cooper. He’s absolutely amazing. An early safety champion and pioneer and a legend in anesthesiology, even though he’s not a medical doctor, Anesthesia was early, I’m talking about the late 1970s in owning its safety problems and adopting a scientific approach to safety improvement. Today, it seems to still be the only specialty that is the demonstrably, dramatically safer and has helped make other specialties safer through their simulation centers.
So you’re all physicians, Dave, you’re an anesthesiologist, hurrah. And so many people who’ve been active with us in healthcare reform, a disproportionate number are from anesthesia. Carolyn you’re an internist. And Ken, according to your bio you’re board certified in six specialties… you’re the only doctor I would need for my whole life cycle! So could you guys tell me what holds the other specialties back from anesthesia’s full court press? So, Carolyn and Ken, I think you’re best prepared to answer, what’s holding the others back?
[00:14:28] Carolyn Clancy: Well first we should all applaud what the field of anesthesiology did. I would also argue that they had something of an easier target, right? I mean this is a field that uses a lot of machines. This is a field where many anesthesiologists would go from one OR (operating room) to another. So standardizing how all the machines worked and so forth and standardizing the procedures made infinite sense. And frankly, I would think it gave them a lot more flexibility.
I would also say that the surgeons are not that far behind anesthesia, probably by a number of years, but really coming out of VA with the National Surgical Quality Improvement Program which was then exported to private sector hospitals some years later. Internist are somewhat different, right? There are certainly procedural internists, but it is a sort of different type of work. And I think if there’s one thing that we’ve learned over these years, it’s that improving patient safety is a team sport. So I sure want to keep applauding what anesthesia did, but no specialty or individual group of physicians can do it alone.
What one might also argue that the anesthesiologists who are utterly brilliant in avoiding some of the tougher problems, like conversations with surgeons, about what time does surgery start and lots of well-known tensions in that setting and so forth. All of which are amusing and part of the background, unless they impact how safe the care patients get.
[00:15:59] Ken Kizer: A couple of things to that. And I don’t think we should lose sight of the fact that one of the reasons anesthesia responded so early and so forcefully was it was also facing an existential crisis from the malpractice problem that it had. And so, it had a real incentive, unlike almost no others – perhaps OB/GYN faced a similar crisis, not long afterwards – that was a powerful driver for what anesthesia did and what then became part of its culture and has continued to this day as being a core part of its culture. The progress has been made in other areas as Carolyn noted, much of my clinical work in the past was in emergency medicine. And I know emergency medicine has really made a lot of progress.
Sometimes it’s hard to assess that because the baseline data where they started from isn’t known. So it’s hard to assess where we are today not knowing exactly where we started from. But I know certainly how emergency medicine is practiced today with an eye towards safety is very different than it was when I started out in the field in the late 1970s. So I would think it’s come a long way and I know others have made the same statement. Although that progress does seem to – as you noted Karen – seems to have perhaps stagnated a bit across all specialties.
[00:17:27] David Mayer: Karen, it might be helpful to provide our listeners with a little background. The Anesthesia Patient Safety Foundation was founded in 1985. After a prime time television show highlighted four horrible deaths related to anesthesia. As a specialty, it was embarrassing to watch, but I believe most importantly, our leadership showed that they weren’t in denial and took the safety issue seriously. At that time, when you looked at mortality studies, they showed that you had a one in 10,000 chance of dying due to anesthetic-related error or complication.
The Anesthesia Patient Safety Foundation used very early outcomes data, but most importantly, closed claims data to identify the top areas to begin focusing in on. Things like unrecognized, misplaced endotracheal tubes, when a breathing tube is mistakenly put into the esophagus versus the trachea. Unrecognized hypoxic mixtures that are being given by anesthesia machines. Unrecognized disconnects between our endotracheal tubes and our breathing circuits. All these things were happening, and we had no warning or clue if they were going on and when they were going on.
A true partnership was created and within industry to try to help solve these issues from the work came numerous clinical improvements, things like pulse oximetry, capnography, fail safe systems, and anesthesia machines that prevented the inadvertent giving of a hypoxic mixture. On the pharmaceutical side, safer anesthetics with less side effects went into production and research and came to market. It wasn’t only just machines and tools and pharmaceuticals, but things like hand-off of care, training and checklists also originated within the anesthesia community.
Karen mentioned the great work of Jeff Cooper, a great pioneer and true safety leader. Jeff along with Dave Gaba and others embraced simulation and created training programs that not only improved our clinical skills, but also those softer skills we hear about. Team-based learning leadership communication-based skills, similar to what was done with crew research management applications in aviation. And to show the success of all these efforts. The last data I have seen showed that the chance of having an anesthetic-related complication or death from a complication is one in 450,000 per anesthetic. So that’s one death in every 450,000 anesthetics compared to one death in every 10,000 anesthetics over 30 years ago. We’re as close to Six Sigma as any specialty in medicine. And I know this model has been embraced and it’s starting to be rolled out in other specialties, but I think it’s a true case study of how to apply partnerships and not only use skills and techniques, equipment and machines, but also to use the softer skills of communication, team-based learning, and leadership like aviation does.
[00:20:57] Karen Wolk Feinstein: Thank you all for your comments and in particular, thank you, David, for all that insight and background. We applaud the absolutely amazing work of our colleagues in anesthesia and hope that they’ll have an even greater influence in safety and other specialties. As I mentioned earlier, if you’re interested, if you want to learn more about anesthesia’s pioneering work, I would encourage everyone to listen to our anesthesia episode with doctors Jeff Cooper and Aman Mahajan. Marty, I’m turning this over to you for the next question.
[00:21:33] Marty Hatlie: I would like to return to the theme of leadership. So again, going back to the beginning of this movement, shortly after the IOM report came out, we saw just huge leadership step forward. The Veterans Administration, actually Ken, when you were there and even before the IOM report, but certainly afterwards. AHRQ under John Eisenberg and then you Carolyn, the CQuIPS, the National Quality Forum, the Leapfrog Group and NCQA, they were all influential organizations that jumped in early. And for quite a while, there was this national interest and energy and it felt like a real movement that would produce the results.
Ken, I think you and I authored an article with George Lundberg and other leaders, Lucian Leape, Don Berwick, saying, “this is the number one priority.” So we’ve had a lot of leadership I think, and yet we haven’t seen the results we expected. And flash forward 20 years, we have the National Academy of Sciences now weighing in with a report last year, Paul Tang led the committee that developed it, saying that patient safety was at a relative standstill in this country. And many other reports that have kind of found similar findings in the last year.
So I’d love your thoughts, what happened? What, why wasn’t leadership and medicine enough to kind of produce the outcomes that we expected. Carolyn, why don’t we, again, start with you.
[00:22:49] Carolyn Clancy: It’s a really, really important question, because I’ve heard this refrain a number of times. I think what has changed is not actually the amount of work going on to make care safer. And I say that through leading the panel of people who judged awards for the awards given by the National Quality Forum and the Joint Commission every year in the name of John Eisenberg. And I have to say that some of the work that is submitted is completely breathtaking in its scope and what it’s trying to do. And what’s really impressive to me is that there’s applications from organizations you never heard of, but who are taking this very, very seriously. I think what has died down is the public noise. You know, at the time this was made very, very tangible to the public as in it could happen to you.
So in a funny way, although the work has – it emerged and continued to develop – the clear message to the public about what you can do I think has become much more muted. And what you can do and why you should care and how this would impact your decisions. I think that we do need more work in that area.
[00:24:00] Marty Hatlie: Dave, what do you think?
[00:24:03] David Mayer: Well, I first, I totally agree with Carolyn about some of the work that’s being done out there is truly breathtaking and there is some great innovation that continues, but I want to refocus this question a little bit, Marty, and we spend a lot of time talking about patient safety. But many of us including everybody in the panel here believes that there’s a bigger problem.
We know the healthcare system is not safe for those receiving care, but it’s also very dangerous for those that are providing care. Lucian Leape and Paul O’Neill told us many years ago, we can’t have achieve optimal patient safety without striving for an optimal workforce safety. Before the pandemic, workplace injuries, burnouts, depression rates, and suicide were higher in health care than almost every other industry and the pandemic has only made things worse. It’s exposed many of these deficits and dangers to our caregivers.
One of the things that scares me the most is workplace violence. We’ve seen three, four times increases in hospitals of workplace violence affecting the frontline workers. This isn’t just occurring on airplanes. It’s occurring in emergency rooms and hospital lobbies and on floors within hospitals. And it’s my belief that hospital leaders need to have more of a comprehensive approach so the safety of the healthcare system as a whole, including those that provide care and those that receive care. And when we figure that out together, I think you’ll see some things move quicker than they have in the past.
[00:25:40] Marty Hatlie: Yeah, thanks Dave. That’s a really provocative thought. I do a lot of work with consumers in this space and it often feels like we’re on different teams. Like there’s the provider team and the consumer team. Why is that when everyone’s at risk, when systems are unsafe? So I’m hoping that is a collateral benefit from the risks that we see so clearly now that providers have. Ken, what are your thoughts on this question?
[00:26:07] Ken Kizer: I would agree with what both Carolyn and David had have said as well. I think that it’s hard for the professional community because there are so many other issues that have come and assumed front page. Certainly, COVID has topped everything in the last couple of years but even before that, there were all kinds of other things that achieve center stage for a lot of people. Both in and outside the profession people are asking, why should this continue to be a top line issue? And perhaps we haven’t done a good enough job in communicating to them that the problem still exists and that there are solutions that could be taken that would reduce the problem. Hopefully we’ll get to some of those later, but. I don’t think that it has remained the center stage issue, certainly for the public and for their elected officials, that it was 20 years ago.
[00:27:03] Carolyn Clancy: Marty, if I could just jump in for one second, the one thing I would say is, Ken is so on point about other issues being distractions. The pandemic has really highlighted very, very important issues of safety. To Dave’s point, think about all of the campaigns there were to make, buy, find unforgotten warehouses full of personal protective equipment. A lot of concern about that. A lot of concern about the safety of caregivers and family members with a household member with COVID, right? How do you take care of somebody like this at home?
A big challenge that continues to this very day and most tragically we saw horrendous number of deaths in nursing homes and other congregate settings. We’ve learned a lot from that and it is my highest hope that we can learn from that and link that more directly to all the work that we’ve tried to do in safety before. This is not unique to COVID, but it is part of what we need to improve in healthcare moving forward.
[00:28:05] Marty Hatlie: Thanks Carolyn, and I just want to comment too that one of the things that’s happened over the 20 years is we’ve have seen this shift from hospitals to other settings, including home. I mean, it’s not only continuing at home, but there’s more and more care happening at home and in long-term care. So it’s almost like the complexity is increasing as we keep fighting the fight.
[00:28:23] Carolyn Clancy: Absolutely.
[00:28:24] Marty Hatlie: Okay. Karen, I think you’ve got the next question.
[00:28:27] Karen Wolk Feinstein: Yes. And I just, another comment of the last conversation, we talk a lot about distrust. We can see distrust everywhere, but certainly patient harm is a source of distrust. Let’s look at one last question about leadership. Ken, in my mind, you’ve always been out there, out front in patient safety and if I’m right, you set up the VA National Center for Patient Safety in 1998.
What emboldened you to be such an early and effective advocate? And also, I am sure you got some pushback early on. You were exposing a problem that had laid buried for a long time. What obstacles did you encounter and how did you ever have the courage to come forward?
[00:29:20] Ken Kizer: Well, thank you for the kind words and for the question, I think there are several things that I would say in response and creating the VA National Center for Patient Safety was one of a half a dozen or more things that we were doing at VA. We’ve created the National Patient Safety Partnership and a number of other things during the 1990s and fundamentally, it was because it was the right thing to do. And I think that’s what many of us in healthcare are driven by is the opportunity to do the right thing. And I had a position and the opportunity to actualize that. And so tried to run with it.
Now, I should tell you as far as opposition, when I was discussing this with – what I proposed to do – with the secretary and in turn the White House, their comments were very straightforward. I mean, the secretary was clear, he said, “you know, I kind of understand what you’re doing. My wife’s a nurse and she tells me about all these bad things that happen. And so I get it, but you understand this is political dynamite and that if this goes the wrong way, you’re the first casualty.” And so as long as the rules of engagement were clear, I said, “okay, I understand.” And we moved forward. There were a couple of other things I think that influenced my commitment, if you will.
One was when I was the director of health for California for many years before I went to the VA. And I saw this stuff happening all the time in private hospitals and indeed one of the questions that I often got when I went to the VA is “isn’t this all different?” And I said, “no, the main difference between the VA and the private sector is that things, everything is made public in the VA. In the private sector, it’s all secret and you just don’t hear about it, but the same stuff is going on all the time.” As a licensing official for the state, I saw this stuff happening all the time. The other thing that that actually did influence my thinking significantly was my wife in terms, she was a type-one diabetic and had essentially every complication that a type-one diabetic could get.
And so there was a lot of opportunity to interface with the healthcare system over the 40 plus years that we were married. And I saw these things happening in her care. So, it wasn’t just professional, but it was also personal. And indeed there’s somewhat some irony, I suppose, that as the person who coined the term “never events” my wife had it at least twice that significantly contributed to her ultimate demise. So, it was, I think the combination of knowing the problem, knowing it well, seeing it personally, as well as professionally, and having the opportunity to do something about it and really not caring whether I was the first casualty or not. So, you know… it worked out.
[00:32:29] Karen Wolk Feinstein: Well I’m so sorry to hear about your wife, probably good for the world that you took a tragedy and at least turned it into this passion for improving safety and healthcare. And reducing never events, but we still have a lot of work to do. I’m struck that over the last two years, we’ve at the Foundation have been working and build a coalition to work in the policy arena, trying to apply lessons that we learned from maybe aviation transportation and other industries with steady progress.
And it led us to support the idea of a National Patient Safety Board that would be modeled after the National Transportation Safety Board, because it seemed to be the missing component. And I say, what do other industries have? They’re so much safer, what don’t we have?… We don’t have one federal agency solely focused on safety and particularly coming up with solutions. My latest interests are autonomous solutions that use technology to take the burden off the front line. There’ve been outstanding leaders in health reform for over like three decades who keep recommending this, but it never gets done.
So Dave Mayer, you’ve been one of those outstanding leaders. I know the Patient Safety Movement has been passionate. Talk to me about why can’t we get this done.
[00:33:53] David Mayer: Well, thanks, Karen. I’ll start with just over a year ago when I was still the CEO of the Patient Safety Movement Foundation, we made a call for what we term the patient safety moonshot. The concept of achieving zero preventable deaths by 2030. We have great examples when we put a stake in the ground and work together with a common goal. We have seen great things happen when we’ve done that, putting a man on the moon, curing polio, and we thought that sort of initiative and rallying around a concept would be very beneficial. Besides so many other areas of focus within this arena, we felt there were three key areas that needed to be addressed.
And you took the lead, you and the Jewish Healthcare Foundation, on what we strongly believed in and that was the creation of a National Patient Safety Board. We’ve seen examples of this in children’s hospitals and others now that are showing that shared learning and machine learning and data and using it the right ways can move forward and improve care and save lives.
So the first of the three things was the creation of the National Patient Safety Board. The second, we felt that incentives had to be aligned with the quality and safety of care being provided, not the volume and quantity of care that’s being provided. And that still exists all too often in healthcare today. And the third major component we believed was transparency.
We needed to embrace the concepts of transparency throughout the healthcare system, learning from our mistakes, feeling comfortable to raise our hand when something doesn’t feel right, all those concepts of outcomes and transparency. And so I know that the Patient Safety Movement Foundation and many others have strongly supported the work you and the Jewish Healthcare Foundation in calling for the creation of a National Patient Safety Board. So kudos to you, Karen, and we’re behind you all the way.
[00:35:53] Karen Wolk Feinstein: Let’s hope maybe 2022 will be our year… we’re trying! Now to turn this over to Marty.
[00:36:00] Marty Hatlie: Well, Karen, I want to just underscore that we have two panelists here, Ken and Dave who’ve experienced loss in their own family from unsafe care. And it just kind of underscores the point that the line between users and providers of care is pretty ephemeral. We all should be on the same team because it touches all of our families. So thank you for sharing that today, Ken, I appreciate it. I didn’t know that about your family experience. But anyway, another mind-boggling gap for us and Karen, this also gets to your point about why we are not hearing more from sort of an organized patient community is, I think they’re confused.
After 20 years, I think they don’t know who to report to when something happens. Our whole reporting system seems very haphazard to them. When I talked to them, they said, “there’s nobody in charge. We don’t know who’s in charge of patient safety in this country… is it CMS? Is it CDC? Is it the Joint Commission? Is it somewhere else?” And we’re still not doing a good job of sort of collecting and aggregating data. Preventable harm is not captured in death certificates… well, sometimes it is, but not consistently. Even CDC says that nursing homes in many states don’t have to report infections, there’s legislation pending about that. There’s still wide variation in reporting requirements in ambulatory care and other settings, and also from state to state.
Ken, you were an early leader in this space in your role at NQF… one of your first major accomplishments that I remember was the never event list that it was adopted and used widespread. So when you look back 20 years and see how that was used and how perhaps how it wasn’t used… what are your thoughts on how we can improve reporting so that we can actually measure progress against some kind of a baseline that we can have faith in is kind of giving us the data we need?
[00:37:46] Ken Kizer: A couple of things. I think the idea of a National Patient Safety Board, which I support wholly, that has to be premised on mandatory reporting. The reporting that provides the grist for the aviation safety reporting board or the National Highway Traffic Safety Administration. What they do is based on mandatory reporting of events that occur. And as you know, Marty, for I’ve been a long-time advocate of, of national reporting of patient safety events, the never events as a good list to start from. There are some version of that now enacted in about 29 states which means that there’s another 21 where there’s no reporting at all.
But the problem is that those lists often are codified in statute. So, the never event list – if you want to call it that, technically serious reportable events – has changed four times, we’ll probably change again before too long. And as it changes, the state reporting requirements haven’t changed with it. So those states that adopted the first list or the second list, they’re not necessarily comparable and you have all kinds of variations across the state. So you really can’t compare to what’s occurring in different states because the data’s just not comparable. And the solution, the, the obvious solution is that there should be national reporting and that list should be kept current and updated, and it should be a mandatory requirement that these events get reported.
Even in the states where there is reporting. We know that it’s extremely variable. Some hospitals report frequently and assiduously, others don’t report at all. And there really isn’t any consequence for not reporting. So again, I think the solution is mandatory national reporting.
[00:39:44] Marty Hatlie: Ken, do you see that happening? Do you have a place in mind? Do you think you see that happening at CDC or a CMS or a new place?
[00:39:51] Ken Kizer: Well, I think where the repository of the information is could be any number of places, CDC is fine, it could be at HHS or it could be at other places as well. I think that’s a minor issue relative to getting the legislation enacted that would require the reporting in the first place.
[00:40:13] Marty Hatlie: Ken, I’m going to share an anecdote with the group, but I’m from Minnesota, which was one of the first states to do never event reporting and after my mother grew her children, she became the church secretary. And every year when the report came out, she would put it in the church bulletin, and she got the spin, right because she said she would remind people or have the priest remind people. These are the good hospitals. These are the hospitals that report. This stuff happens everywhere, but these are the hospitals that we can trust because they’re transparent.
So I think they did a good job actually in Minnesota, really getting that message out in the public that this does happen everywhere. It could happen in good hospitals as well as bad, but these are the ones that are responsible and reporting it forward.
[00:40:50] Ken Kizer: Yeah, I joined with the governor in making that announcement when Minnesota initiated reporting.
[00:40:57] Marty Hatlie: Well, clearly my mother had our lady of the lake and mom in Minnesota heard you or heard that and followed through as an acolyte.
[00:41:04] Karen Wolk Feinstein: Marty, I just wanted to say, I guess you have to have a sense of humor or understand why people don’t trust government reporting, but in Pennsylvania, in the summer of 2020, the cumulative, the total number of COVID deaths actually declined.
So I asked the secretary of health, “how do you get undead? Because I really want to figure out how to be undead.” She said, “oh, well you just change the criteria of what a COVID death is.” So in the middle of the summer, they changed the criteria and suddenly people undied and you worry a lot… But I also have to say with the airline industry, the one thing that I think is really positive is when they formed ASIAS, every airline signed on and agreed it was in their interest to give the most accurate, open, rapid data possible because they saw as an industry that everybody would benefit if they got safer. And I still fear that we haven’t quite gotten there yet. Thanks, Marty, go ahead.
[00:42:06] Marty Hatlie: Okay. So this is really our last question. So it’s an opportunity for us to kind of collect our thoughts with some closing comments – or lead us into that at least – we’ve mentioned several times in the course of this conversation that patient safety seems to have lost its mojo, at least in the United States. We actually see some very strong leadership out of the World Health Organization, just last year, calling on countries to prioritize this, but in the United States, we’re just not hearing them about it as Karen has mentioned. It’s not in the Biden Administration’s draft strategic plan. We’ve filed comments about that and there’s dialogue happening there.
As Carolyn mentioned, consumer advocates seem less insistent, less loud about this. Obviously, there’s a lot of other competing priorities and I’m at a point as a person who identifies primarily as a patient advocate, that the average system doesn’t even have medical safety on their radar. So how do we get looking forward to shifting from the past 20 years to perhaps the next 20 or 10 cause they’ve got a ten-year plan. How do we get organizations and individuals to care enough, to demand change, or to at least choose the safest providers and what will get kind of the attention that we need to the WHO plan or AHRQ has a plan? IHI has a plan to really make this again, prominent in sort of the American medical sphere. Carolyn, why don’t we start with you?
[00:43:27] Carolyn Clancy: So it is really, really a great question. By definition, our healthcare system is public and private. The government has a very substantial role, but the private sector does as well. So I think that that kind of approach to partnership would need to be sort of the way to go. Just picking up on Ken’s earlier point, transparency can be painful at times, but I think it has been very, very good for VA. So to this day, if a patient is harmed under our medical care, that is immediately disclosed to the patient and family. This is presuming that the patient survived and with an apology and a commitment that we will do better about that in the future. That is not something that happens across the healthcare system. But I do think that transparency has got to be linked with effective strategies for what do we do about this.
To that extent, I would say that Partnership for Patients was a real beacon coming out of CMS, but I think what really drove it was a very, very strong public-private collaboration with the LAN Network, constantly sharing lessons about what works, what didn’t and so forth. It’s complicated business and so balancing short-term wins with the longer-term improvements that we need to make is going to be a very substantial challenge here. I think we’re up to it. I think in reviewing lessons from this pandemic, which is top of mind for everyone right now, that’s going to give us a real boost to think about this topic in a more meaningful way, because it’s something everyone can understand and has experienced in some fashion.
[00:45:08] Marty Hatlie: Supply chain is a safety issue.
[00:45:09] Carolyn Clancy: Totally! A safety issue and we have now an occupational safety and health administration, really taking a very, very strong interest in the safety of healthcare workers, which is new and usually important.
[00:45:22] Marty Hatlie: Dave, I feel like you’ve already kind of weighed by saying the connectivity between provider safety and worker safety and patient safety is there, but what more would you add?
[00:45:34] David Mayer: Marty the only thing I’ll add is, I guess as I’ve gotten older and reach this age, I’ve become a little more cynical. And sometimes I feel like George Carlin during a standup comedy act or something, but my gray hair has taught me that for many, healthcare is still a business. And there are many stakeholders that are out there that like the current state, they think everything’s fine. Healthcare is doing well. And why do we want to change it?
We’ve had many pushbacks when we’ve been trying to get legislative discussions or initiatives going forward by lobbyists for many of the large organizations in healthcare who don’t want to see change, they want to keep the status quo. And so maybe that’s my gray hair talking or 30 years of trying to create change, but I still believe we got to continue to fight, but it’s going to be an uphill battle to get any effective changes done with all the different priorities being distributed around and issues that administrators have to face. So that’s the last I’ll say about that.
[00:46:43] Marty Hatlie: Ken?
[00:46:45] Ken Kizer: Well, I would agree with the other comments that have been made. I think if we… the comments that were made earlier about how do we get the administration, current administration, more focused on the issue, and include patient safety more prominently in some of the plans and agendas going forward. And I think the COVID pandemic and all of its ramifications and complexities provides a lot of opportunities to highlight and showcase this issue. And I guess I would revert to one of the fundamental maxims in patient safety is, “make it easy to do it right and hard to do it wrong.” So as far as how do we get the administration engaged, we need to find ways to make it easy for them to do what’s right and focus on that.
[00:47:46] Marty Hatlie: Thanks, Ken. And Karen, I’ve seen you nodding as each of our presenters have given us their thoughts. I’d love to hear from you. I know you think about these issues too, and I’m going to pass it back to you with the opportunity to either comment or make some closing remarks.
[00:48:00] Karen Wolk Feinstein: Well thank you. I have to say what a privilege it is for me to be here today with Dave and Ken and Carolyn and Marty, you’ve all devoted careers to safety and become somewhat legendary in this field. And I’m delighted to be able to share an hour with you. And I thank you for being here. I would just say that I always joke that I’ve played the whole xylophone of safety solutions and I’m looking for another note that might add to the music. And I really am somewhat excited about the possibilities of a National Patient Safety Board, if among other things, just collecting all the things we know that work and coming up with an ongoing outpouring of good solutions… it’s just time.
And I would add to that things have changed a lot. My involvement began in ’97, ’98 and there wasn’t a lot of safety technology around, but now I’m sitting here in Pennsylvania and we have 18-wheel semis barreling down our turn pipe without a driver. Technology has really advanced in the field of safety. And I say, “let’s go for it. Let’s start applying it the way other industries have.”
So anyway, if any of our listeners want to learn more about our efforts to establish a National Patient Safety Board and what it could be and what it isn’t. Please visit npsp.org. We also welcome any comments and suggestions you have. If you found today’s conversation helpful, please share it or any of our other podcasts with your friends and colleagues, we can’t improve the effectiveness of our healthcare system without your help. You, our listeners, friends, supporters. You’re in a central part of the solution. So let’s go forward.
I know this is going to be – Dave, you’re not exaggerating. You’ve walked 3000 miles – but I know how much everyone here cares. I think people who are listening to these podcasts care and let’s find a way to make progress in 2022. One thing we know the pandemic has been a setback. We have less safety than we had before. So hopefully that will motivate ourselves and others. Thank you all.
If you want a transcript or the show notes with references to related articles and resources that can be found on our website npsb.org/podcast/. Up Next for Patient Safety is a production of the National Patient Safety Board Advocacy Coalition in partnership with the Pittsburgh Regional Health Initiative and Jewish Healthcare Foundation.
It is executive produced and hosted by me Karen Wolk Feinstein. Megan Butler and Scotland Huber are my associate producers. This episode was edited and engineered by Jonathan Kersting and the Pittsburgh Technology Council. Thank you, Tech Council! Our theme music is from shutterstock.com, social media and design are by Lisa George, and Scotland Huber. Special thanks to Robert Ferguson and Steven Guo. Thank you all for listening.
—
Subscribe on your favorite podcast app: Apple Podcasts | Google Podcasts | Spotify | Pocket Casts
