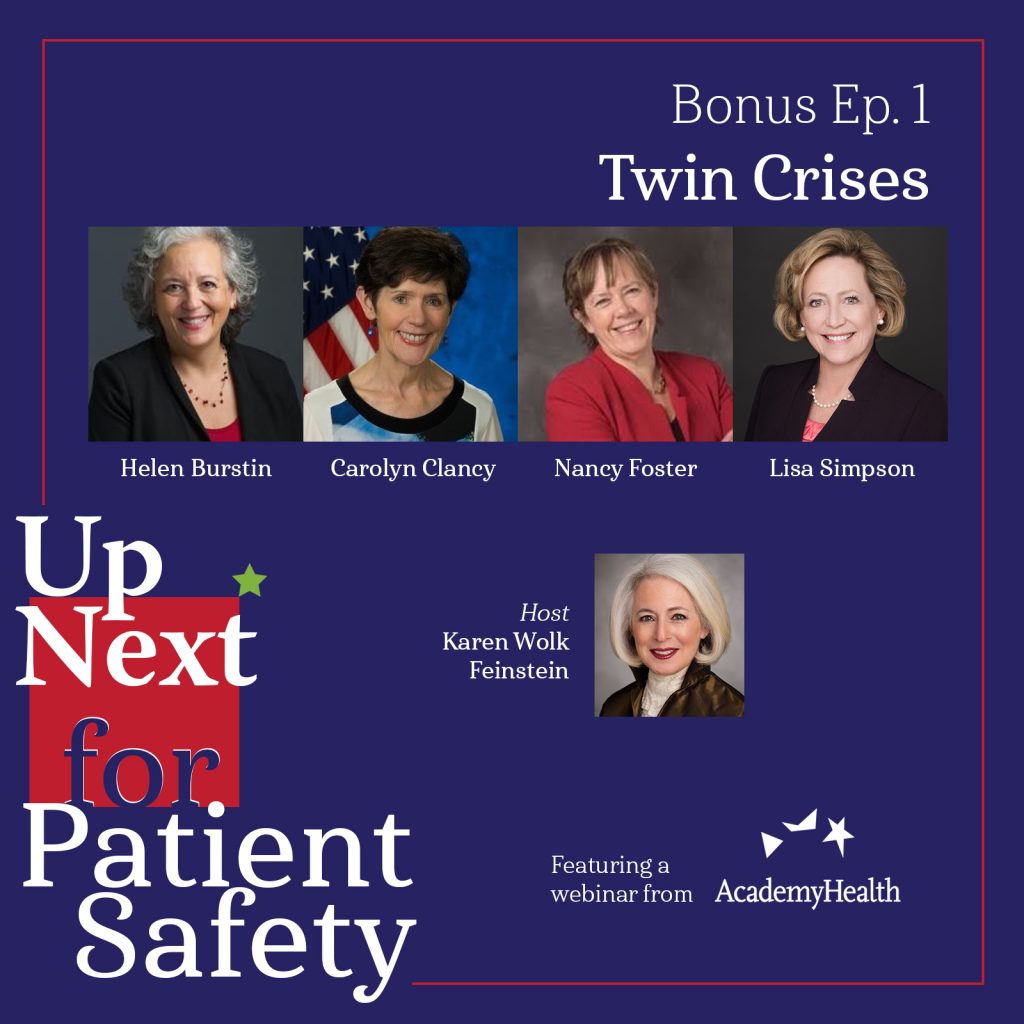
Bonus Episode 01: Twin Crises
How are the “twin crises” of medical error and the departure of experienced clinicians from the workforce threatening the safety of health care? What solutions for patient safety are possible in these uncertain and unstable times? In this special podcast episode revisiting an AcademyHealth webinar, join host Karen Wolk Feinstein as she moderates a conversation with four of our nation’s pioneer leaders in healthcare safety research and policy: Dr. Helen Burstin, chief executive officer at the Council of Medical Specialty Societies; Dr. Carolyn Clancy, assistant undersecretary for health for Discovery, Education & Affiliate Networks at the Department of Veterans Affairs; Nancy Foster, vice president of quality & safety policy development at the American Hospital Association; and Lisa Simpson, president and CEO of AcademyHealth.
Listen to this episode on: Apple Podcasts | Spotify
Featured Speakers
- Karen Wolk Feinstein, PhD, President & CEO, Jewish Healthcare Foundation & Pittsburgh Regional Health Initiative
- Helen Burstin, MD, MPH, Chief Executive Officer, Council of Medical Specialty Societies
- Carolyn Clancy, MD, Assistant Under Secretary for Health for Discovery, Education and Affiliate Networks, Veterans Health Administration
- Nancy Foster, Vice President of Quality & Safety Policy Development, American Hospital Association
- Lisa Simpson, MB, BCh, MPH, FAAP, President and CEO, AcademyHealth
Referenced Resources (in order of appearance)
- Surveyed nurses consider leaving direct patient care at elevated rates (McKinsey & Company, 2022)
- Clinician of the Future Report 2022 (Elsevier, 2022)
- Health Care Safety during the Pandemic and Beyond – Building a System That Ensures Resilience (The New England Journal of Medicine, 2022)
- Why Health-Care Workers Are Quitting In Droves (The Atlantic, 2021)
- AcademyHealth Webinar: Patient Safety and Health Worker Retention – Twin Crises (AcademyHealth, 2022)
- Health workforce shortages begin to weigh on patient safety (Axios, 2022)
- Beyond ‘John of AHRQ’ – John Eisinberg at Penn Medicine, Wharton and LDI: A Profile of One of the True Greats of Health Services Research (University of Pennsylvania, 2017)
- Digital Healthcare Research: Program Overview (AHRQ)
- Clinical Informatics and Patient Safety at the Agency for Healthcare Research and Quality (Journal of the American Medical Informatics Association, 2002)
- 10 Patient Safety Tips for Hospitals (AHRQ, 2009)
- The U.S. Agency for Healthcare Research and Quality’s activities in patient safety research (International Journal for Quality in Health Care, 2003)
- To Err is Human: Building a Safer Health System (IOM, 2000)
- National Institutes of Health Buildings and Facilities: Congressional Justification FY 2023 (U.S. Department of Health and Human Services, 2022)
- About CAHPS: Consumer Assessment of Healthcare Providers and Systems (AHRQ)
- Agency for Healthcare Research and Quality Fiscal Year 2023: Justification of Estimates for Appropriations Committees (U.S. Department of Health and Human Services, 2022)
- Friends of AHRQ Coalition (AcademyHealth)
- Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS): Patients’ Perspectives of Care Survey (CMS)
- Computerized Provider Order Entry: The Basics (HealthIT.gov)
- Trends in Adverse Event Rates in Hospitalized Patients, 2010-2019 (JAMA, 2022)
- A nurse was just sentenced to 3 years of probation for a lethal medical error (Vox, 2022)
- Fifteen years after To Err is Human: a success story to learn from (BMJ Quality & Safety, 2016)
- About Learning Health Systems (AHRQ)
- National Action Plan to Advance Patient Safety (IHI)
- Aviation Safety Information Analysis & Sharing: Overview (FAA)
- Data Modernization Initiative (CDC)
- Network of Patient Safety Databases (AHRQ)
- Office of Inspector General Report on Adverse Events in Hospitals: A Quarter of Medicare Patients Experienced Harm in October 2018 (U.S. Department of Health and Human Services, 2022)
- Peer Review of a Report on Strategies to Improve Patient Safety (National Academies Press, 2021)
- United States Core Data for Interoperability (USCDI)
- USCDI+
- Fast Healthcare Interoperability Resources (FHIR)
- AHA Question for Quality Prize (AHA)
- Uncaring: How the Culture of Medicine Kills Doctors & Patients (2022)
Episode Transcript
[00:00:00] Helen Burstin: But I think we’ve collectively, sometimes spent too much time sort of admiring the problem and not getting to solutions as quickly as we needed to…
[00:00:14] Carolyn Clancy: We just cannot see a lot of instances of harm. And I think that’s something we’re gonna rue the day for…
[00:00:26] Lisa Simpson: But an actual national action plan on patient safety data? We don’t have one…
[00:00:34] Nancy Foster: We need that independent validation of what are the important, critical things to move forward in your institution now in order to advance safety…
[00:00:47] Karen Wolk Feinstein: Welcome to a bonus episode of Up Next for Patient Safety. Our nation faces an urgent need to address twin crises in healthcare, which are inseparable. Our medical error rate is rising because experienced nurses and doctors are leaving the workforce and we’re losing our frontline nurses because our medical error rate is soaring. Committed professionals don’t want to do harm, but it’s a challenge to provide safe care when trusted and experienced colleagues are no longer there. These twin problems preceded the pandemic, but they’ve gravely worsened during the past two years. Recent reports from the New England Journal of Medicine, the National Academies of Sciences, Engineering, and Medicine, and the American Nursing Credentialing Center substantiate this. No healthcare system, hospital or nursing facility has escaped healthcare’s great resignation.
In this special podcast episode, we share a recent webinar moderated for AcademyHealth that features four of our nation’s pioneer leaders in healthcare safety research and policy. We discuss why we failed for more than two decades to significantly reduce medical errors and what solutions for patient safety are possible in these uncertain and unstable times. Here is our deep dive into Patient Safety and Health Worker Retention: The Twin Crises.
Hello everyone. I’m Karen Feinstein, President and CEO of the Jewish Healthcare Foundation and the Pittsburgh Regional Health Initiative. I’m going to serve as your moderator today. We’re going to be talking about the Twin Crises, our diminishing workforce and our increasing rate of medical error and adverse events.
These two crises are not unrelated. In fact, we think they’re sort of mutually reinforcing, unfortunately. So with four distinguished panelists, we’re gonna look back and we’re gonna look forward. I am very much looking forward to this conversation because we’ve gathered here when I consider a dream team or as I affectionately regard them, John Eisenberg’s AHRQ Angels – though Carolyn Clancy actually succeeded John – to consider these issues. I met all four women when they served in key roles at the Agency for Healthcare Research and Quality, which we all refer to as AHRQ though they were there for different terms during critical years, 1995 to 2013, when our hopes and aspirations for advancing patient safety were at their peak. All four have gone on play key roles at other organizations.
Dr. Helen Burstin served at art from 2000 to 2006. She’s now the CEO of the Council of Medical Specialty Societies after serving as Chief Scientific Officer at the National Quality Forum. Dr. Carolyn Clancy served as AHRQ director for 10 years, from 2003 to 2013, after serving as CMO and executive-in-charge of the Veterans Health Administration. She’s now the Assistant Under Secretary for Health, for Discovery, Education and Affiliate Networks. Nancy Foster served as the AHRQ Director for Quality Improvement Activities for five years from 1997 to 2002, and now serves as Vice President for Quality and Patient Safety Policy at the American Hospital Association. And last, but definitely not least, Dr. Lisa Simpson served as the AHRQ deputy director for seven years from 1995 to 2002, and now serves as President and CEO of AcademyHealth.
So welcome everyone. We’re very anxious to hear from you. So, my first question to all of you, during your time at AHRQ, what was your greatest accomplishment? And on the other hand, what do you wished you accomplished that you didn’t? I’ll just go in alphabetical order, Helen.
[00:04:48] Helen Burstin: Well, thanks so much for organizing this. It’s really a treat to be on a call with so many of my heroes and friends. Um, so I’d have to say one of the things I think collectively was one of the greatest accomplishments that I had a chance to be part of was actually the launch of the Health IT and Patient Safety portfolio at AHRQ. I think at the time in the early aughts, it was sort of a twinkle in everyone’s eye about what Health IT could do to transform care and particularly patient safety. And I distinctly remember it was also my first time as a fed, having to come up with an acronym and remember sitting with John Eisenberg coming up with CLIPS. I was very excited that I had my first acronym, Clinical Informatics to Promote Patient Safety. So I think that the idea that we were sort of first out saying, we recognize this as an issue. This is a really important opportunity we should take on. And the amount of money that thankfully came from Congress over a hundred million, I think over a couple of years was exciting. And I think an important issue.
I think I’ll actually stay on that same issue though. I think for the flip side of your question, Karen, of what do we wish we had accomplished, but didn’t, I think AHRQ and we were often first to sort of consider an issue – like sometimes people say admire an issue, like “this is a really big problem. We should do something about this” – and I think in some instances that was the case for Health IT. Like, this is really important. We could really do something here, but I think we’ve collectively, sometimes spent too much time sort of admiring the problem and not getting to solutions as quickly as we needed to. And it’s taken decades still to get to more generalizable solutions in this space. And even then, I still think we have lots of islands of excellence and we’ve not done enough to kind of bridge those and really get to a different level, higher level of patient safety for the nation, so thanks.
[00:06:31] Karen Wolk Feinstein: Terrific observation that I second. Carolyn?
[00:06:36] Carolyn Clancy: Sure. So, you know, one of the greatest things we ever did was almost by accident, and this was really motivated by the folks in our communications team, but we actually distilled a list of 10 things hospitals can do right now to improve patient safety. Now I thought this was very practical and some people would appreciate it. Well, there was this huge outpouring of appreciation and, you know, from very prominent institutions, many of which had researchers that we were funding to do very complicated stuff for the people who were doing quality and safety in real life right now, this was really, really helpful.
In terms of what I wished we’d gotten done… although I could see it then, and it builds a little on what Helen said. I wished we had begun to put in place infrastructure or at least models of same for assessing safety in outpatient settings. We had a run at trying to do this for medication errors and adverse events, because they’re often difficult to disentangle and we were building on the work of a grantee, but we didn’t have the potential to scale it. Some of it is about why Health IT has been so slow and some of it was about other forces, but I think, and I’ll come back to this later, one of our big problems in safety right now is a lot of it is not visible. Because it’s not happening in hospitals, it’s happening outside the hospital, and we don’t have any way to actually see it.
[00:08:13] Karen Wolk Feinstein: Thank you, Carolyn. Nancy?
[00:08:17] Nancy Foster: Thanks so much. I join with my colleagues in saying it’s great to be together again and to talk about patient safety. Thanks so much for making this happen. For me, the most important thing I think I did when I was at AHRQ was to create the first national summit on patient safety to create a research agenda for patient safety. This was in the wake of To Err is Human and President Clinton who was at the time in office saying “let’s get all the federal agencies together and figure out what we can do to advance safety.” We came up with a long list of things we could do to advance safety. But the one that was really intriguing to me was the, to create this national summit, to bring together the federal agencies, to gather ideas from around the country about what could be researched that would drive safety forward in those offices that Carolyn was referring to where they’re overwhelmed with a lot of research, but not clear about exactly what should be high on their agenda.
It worked; it actually became more than a national summit. We had people from the Commonwealth countries coming over. They were excited about the fact that we had $50 million to spend. And that leads me to my flip side in response to your question, Karen. I don’t feel like we solidified and started to really grow the patient safety research portfolio and the budget for it in an effective way. I wish I’d been able to help do that. Um, you know, we had $50 million just by comparison, the NIH this year is spending five times that amount on maintaining their buildings and grounds. Important things to do, but not as important as patient safety. And so really that continuing investment that’s gonna generate a long-term response is what I think we needed.
[00:10:13] Karen Wolk Feinstein: And you and Lisa were there at AHRQ almost the same time. So Lisa…
[00:10:20] Lisa Simpson: Yeah, well actually we all four were there at the exact same time. We overlapped slightly, but we were all there together. So again, I’ll add as Nancy did my thanks to Karen for coming up with this brilliant idea. And I think also for bringing together the very real conundrum of the patient safety challenges we were starting to get into, but also, our healthcare workforce and the burnout and challenges that we are facing and how one is just making the other more toxic. And, so I think this is a really important topic.
In terms of what I’m most proud of, I really turn to the three other leaders on this call in the area of patient safety for their leadership. And so my role there was a little less – was a lot less – visible and substantive, but there’s another effort that’s kind of related, cause I think it’s important also to the future of patient safety. And that was AHRQ’s role in the consumer assessment of health plans survey. And it really, you know, again, um, I – it’s not something I’m very public it’s very publicly known what role I played. But I was, you know, very involved in the launch of that. And I learned, I cut my teeth on a lot of lessons of what it takes to make researchers work together across disparate teams to come up with a unified agenda and just how important it was to give voice to the experience of the patient and the consumer.
And I think we’re in a very different place as a country and as health systems today, but, you know, CAHPS in the late nineties, not even the aughts was really groundbreaking. So I’m very proud of my role in that. On the flip side, I’ll pick up on a point Nancy made and just make it bigger, which is in terms of the funding for research. John Eisenberg, who mentored all of us, you know, we wanted to billionize the agency. I just remember the number of times we ran budget scenarios of how we would do it and blah, blah, blah.
We didn’t achieve that. And we’re still, the agency’s still, you know, not even reaching 500 million in base funding. And I have to say, AcademyHealth runs the Friends of AHRQ coalition, and we’re always advocating to increase AHRQ’s budget. And I think that a substantial commitment to patient safety research and improvement, not just the research, but the data and the skills and the learning systems that are needed to actually translate that research into sustained practice, that’s what we did not accomplish.
[00:12:57] Karen Wolk Feinstein: And, and as one of you said, we’ve little pockets of excellence and they don’t get united or spread and they don’t get sustained. And I often joke. I’ve spent 25 years now on back to baseline. Everything we achieve eventually evaporates because we don’t have that infrastructure. So I remember back in 2002, 20 years ago, we were also optimistic. I think we would’ve imagined that in 2022, we would’ve made great progress.
So let me ask, Carolyn and Nancy, what’s held us back? What forces of resistance didn’t we anticipate?
[00:13:34] Carolyn Clancy: So I’ll mention too, but before I do that, I also wanted to thank you, Karen, because, you know, your work in this area is akin to a force of nature. And just insisting that we keep this on the agenda and you know that the right people coming together can really change the world. So, an inspiration to me, but I think to many others and Lisa, I have to say your role with CAHPS was utterly essential. And I think one thing I’m very proud to have been connected to was pushing HCAHPS, the hospital version.
So I think looking back that we thought Health IT would solve a lot more problems, much faster. You know, at that point in time, there was a lot of excitement about computerized order entry. And to be honest, when I started my career in academia, in the eighties, we had computerized order entry. So it’s not a phenomenally progressive institution, but I just thought everyone did this. You know, that was how it worked, uh, except that wasn’t how it worked.
And I think the what’s held us back are two forces. One is the relentless march, if you will, of care from hospitals to outpatient settings. Now, for many reasons for patients, this is a phenomenally great thing. Who needs to listen to announcements and having people wake you up and you have, you know, very little sense of control. On the other hand, we just cannot see a lot of instances of harm. And I think that’s something we’re gonna rue the day for. Two examples, you know, when I saw an optometrist, I don’t know… a number of years ago when there was a very serious fungal infection reported by the CDC in four patients related to a kind of contact lens fluid.
Well, it turns out the optometrist I see who runs a very small storefront operation had seen two patients in his practice. They were not two of the four, right. There’s no place for that information to go. He, you know, we, he was discussing this as an idle curiosity and I’m thinking, “oh my gosh, that’s two… how many more twos are there?” You know, and there’s probably just so much that we’re not seeing. And the other force I would say is liability. So, on one level we would have meetings about, you know, it’s very important to disclose to patients when something has gone wrong, whether or not that’s obvious to the patient and family. You know, to apologize and to frankly, make a commitment that you’re not gonna do this again. This has been policy at VA since 2008, but by and large it is an outstanding policy in the private sector. Because even when it’s disclosed, it’s like a long, long, long, long time after it happens. Or this is what I hear from patients and families. So, the fear factor related to liability sometimes very real and sometimes not exactly real, I think has been a very, very powerful force.
[00:16:46] Karen Wolk Feinstein: And some recent cases haven’t diminished that fear.
[00:16:52] Carolyn Clancy: Correct.
[00:16:53] Karen Wolk Feinstein: The case we all have been talking about. Nancy, from your perspective?
[00:16:58] Nancy Foster: Thanks Karen. Thank you, Carolyn. That was a terrific important set of two points. First of all, I wanna say Karen, that, that we have seen some progress and in a well-documented study that was conducted with AHRQ funding done by Noel Eldridge for and several of his colleagues and recently published in JAMA. We saw that where focus had been put on things we could measure, we saw significant progress in improving the death rate, improving the harm rate from incidents. That’s great news. The bad news is we don’t have the time, the workforce, or the energy to put all of that kind of energy into every area where we could improve. And there are plenty of opportunities to make care safer. So we have to get smarter about that.
A couple of other things I would mention as inhibiting our ability to increase patient safety. One is the workforce’s concern for personal safety. We know that nurses are injured far too often. I have not in my career heretofore heard so many doctors express concern about their personal safety. We see in the news at least once a week, some group of healthcare professionals being threatened or actually injured in their – in the course of doing their job – that that will definitely detract from people’s ability to focus on patient safety. Secondly, I would point out that we haven’t created this infrastructure that several of us have referred to, to incorporate ideas into practice and to do so with an electronic health record or some other driving force that makes it the easy thing to do.
And so far, the use of EHRs especially around data collection and other things has created more burden than it has saved. And so we have a lot of work to do in order to use that as an effective tool. And then one other, one other point to add to Carolyn’s point about liability is just the individual clinician’s concern how they might be punished as a result of making mistakes. The outcry around the RaDonda Vaught case was so incredible. And I have heard from a number of nurses who expressed personal concern that even in their institution, despite its just culture adoption, they might face, career harm if they were to report an incident, an event. I hope that’s not true, but we have some distance to go before we solve that problem as well.
[00:20:02] Karen Wolk Feinstein: And that case probably poured, what did they say, “Oil on the flame.”
[00:20:07] Nancy Foster: Yeah.
[00:20:07] Karen Wolk Feinstein: Didn’t do anything to diminish the exit from the workforce. So here’s a tricky question, but it intrigues me – I’ve never been able to answer it myself. We can’t blame the media or our academic healthcare publications for skirting the issue of patient safety. I mean, they they’ve done a good job covering it both from, you know, lot of good data and thoughtful research, but also even the sensational and egregious stories. Why can you explain to me, do the public employers, government officials, still seem numb to this problem? I’m gonna ask Helen and Lisa to tackle that one.
[00:20:48] Helen Burstin: I’m happy to start if you’d like, that’s, it’s a really important question. And I don’t know that there’s an easy answer, but I do wanna build on something Nancy just said, cause I think it’s related to this. I think there has been an assumption for too long of an unending elasticity on the part of clinicians – of our workforce. If they could just do more and more and more, and try to address safety, try to do things right, keep patients safe. And I think part of what the pandemic blew up was that concept. And I think we saw, we pushed clinicians past their breaking points. So this idea that if people just worked harder… things would get better. I think it wasn’t gonna happen at all in terms of improving patient safety. I think the pandemic really recognized that.
But I think the other thing I wanted to point out is I think that it is also an issue where I think until it happens to you or a family member, it’s really hard to wrap your arms around this issue. Cause I think to Nancy’s point, it is so diffuse. There are so many different issues really. We call it patient safety, but there’s hundreds, thousands of issues within it that I think it’s hard to wrap our hands around it. Interestingly, if you go to medical meetings, people sometimes ask how many people in the audience have had, you know, you or a family member have had some safety-related issue and every hand goes up and there’s this disconnect then if it’s happening to all of us even, who are probably the most informed, who never leave our loves our loved ones’ bedside cause for fear of what will happen. And you know, when they’re in the hospital, then there’s a translational issue that I don’t think we’ve cracked.
I attended a White House briefing this morning on this new national eradication plan for hepatitis C. There’s something very discreet about, you know, it’s a big issue, but it’s still pretty discreet, right? It’s a condition we can diagnose it, we can treat it. And I feel like that’s been, what’s been really hard on patient safety. I don’t know that because we can’t attack every single aspect of it, it doesn’t seem doable in quite the same way that a clinical issue can be. And I think it’s hard. I think we have examples, really nice examples, like CLABSI, where we’ve made dramatic improvements, but it’s hard to find lots of those examples. And when it’s something, that’s this diffuse, I think it’s just really difficult to tackle it. I wish I had a better answer, Karen.
[00:22:55] Karen Wolk Feinstein: No, I think you brought up a really important point. I was listening last night to Amanpour and they were discussing why so many soldiers in the Russian army now are disobeying orders and showing no interest in continuing the fight. They said, “if you don’t provide people with supplies and backup and, and equipment and armor and what they need, it creates a horrible cynicism.” And I think, you know, for many of our healthcare workers, as you said, particularly during the pandemic, they weren’t given what they need. And even now, you know, the nurses say to us “pizza on Fridays and a meditation room doesn’t do much for the fact that I am frazzled.” I think you hit a really good point at… Lisa do you wanna comment on that?
[00:23:43] Lisa Simpson: Yeah, thank you. I wanna pick up on some of the points that you guys just made. But first let me just say, I think it’s even harder to move beyond that diffuse, you know, to tackle this now than it was three years ago. This is a hugely complex multi-sector, multi-stakeholder, public-private challenge. So I wish it were as simple as Hep C. You know, again, not value one over the other, but this is incredibly complex. And now we’re in a system where the pandemic has not only frazzled our health systems and our health professionals, but the public, I mean, our tolerance for another health challenge, and, you know, we’ve had COVID, now we’ve got monkeypox… there’s stories about polio. I just think the public in general, you asked “why are we numb to the problem?” I think we’re numb generally, because even more so over since the last three years.
But to get back to the point about the complexity, I wanna just, you know, kind of give a few… speak to a few dimensions of that complexity, you know, sustained and fundamental, transformation or improvements in healthcare. I think it’s been when there’s been alignment. So, public and private alignment, external incentives, reward safety improvements, and to do those in a fair way that can’t be gamed – that’s a tall order. When health systems that have the capacity, not just in people, but in systems to you know, provide safe care and that that capacity is continually improved as new evidence emerges and practices are improved. That’s that learning health system concept. When we’ve talked about the clinicians, they’re prepared, and they’re supported in a culture that nurtures the safety for them and their patients. And when patients – let’s not forget the patients in this – are informed and supported for their role to demand no less that they must have safe, respectful care. And then you bring in the equity dimensions and bias and racism in our health system.
Whew. That’s a lot to take on. And so, the question I always come back to is sort of what’s the overarching vision, you know, is there an action plan? Well, there was one developed by IHI in 2020. There have been some before, but that’s the latest and you know, it’s a good place to start, but I always ask. “So what’s the accountability framework for that plan?” It does not lay out who should do what it doesn’t have the agreements of, you know, government, the agencies within government, the American Hospital Association, X, Y, Z, just bring them together. And then what is the strategy for reporting and monitoring progress? And, you know, that’s where I think that is a role of government working closely with the private sector to make that accountability strategy real, because it’s so difficult, the complexity will stymie progress.
[00:26:39] Karen Wolk Feinstein: So, let me ask another question – thanks Lisa – that I can’t figure out. So I sit here in the shadow of Carnegie Mellon University, and we’re gonna have a little Rover riding around Mars soon. We send astronauts to the space station safely. We do mine safety here. We do every kind of safety. We do aluminum manufacturing safety here, and I say to the safety manufacturers, “why not healthcare? Why don’t you put some energy into building our healthcare workers, a safer airplane?” and they say, “there’s no money in our safety products in healthcare.”
This is very discouraging that we don’t see a business model for safety that it’s not built into operations that being safer means that you are gonna be stronger as an organization. What will it take for our industry as a whole, all the players in our industry to align around safety and say, “we have to take advantage of the breakthroughs that other industries have had.”
So, I’m gonna ask Nancy and Carolyn about this one.
[00:27:54] Nancy Foster: Karen I’ll get that one started, you know, it’s a great question. And I will, for one acknowledge that there are significant financial pressures on the healthcare system as a whole on hospitals in particular. The financial picture is not pretty, and you may have seen some of our most notable systems reporting huge losses in second quarter of last year. There’s not a stable financial picture right now. And it could get worse before it gets better is all I can say, but we’re working through it. That can’t impede our efforts to improve safety. We need to focus on that, but I’m gonna take you back to something Carolyn talked about about at the beginning, which is we hear a lot from various folks coming forward and particularly, even when I was at AHRQ and had no ability to buy anything… I was getting information from various people trying to sell me the latest and greatest safety innovation.
It just doesn’t have the same kind of credibility that the list that Carolyn referred to the list of 10 things you can do now, we need that independent validation of what are the important, critical things to move forward in your institution now in order to advance safety. And to really work collaboratively, that enables us to, to stretch across our different institutions and work collaboratively as we innovate, as we install those innovations, in order to really effectively learn from each other and move to take full advantage of what’s coming along. But it’s that, it’s that voice of here are the 10 things to do that we’re missing right now.
[00:29:35] Carolyn Clancy: The one thing we could do right now, wow. This is what makes dealing with Karen, both challenging, but also overwhelming sometimes. I don’t know that there is one thing. At a superficial symbolic level, think it would be phenomenal if every clinician in this country that has to get a license of some sort actually had to sign an annual commitment to provide safe care. Now, on some level, I know a researcher could make an argument that this is meaningless, but that commitment is I believe really, really important. And you know, once a year, every two years, whenever you’re renewing, you’d actually have to think about it. The other suggestion, Karen, is I think we need to figure out how to amplify the voices of people impacted by patient safety.
So I’m not going to suggest that you be cloned, but the notion of challenging others to have these kinds of conversations. We started a bit of work shortly before I left in encouraging patients to report errors – this was in hospital – and it built on a little bit of work that Eric Schneider and others had done when I think he was still with RAND. It really didn’t take off and boy, there was a lot of resistance to this. After all, what do patients know? Well, patients know that yesterday I did not have an IV bag with a red label on it. And today I do, or mom didn’t or whatever Helen referred to, you know, we’re also smart that we actually have people in the room at all times with people that we care very much about, or at least not during the pandemic, but as a general rule… I actually think trying to amplify those voices, whether it’s through dialogue like this, or some other issues because the issue of visibility continues to kind of tear me up.
I have a couple of family members who have been impacted just in this past year by outpatient procedures. Now in neither case, did anyone intend harm? But in one case, the, you know, impact was pretty phenomenal, thankfully, improving now, but if they hadn’t gone back to the same clinicians, they would never know. They absolutely would never know. And in some ways, at least in one instance, I might have advised them to go somewhere else and they were considering that. So I just think that we’ve gotta figure out how to make this more visible. Technically this is not a challenge, right? What’s a challenge is all the competitive forces in our industry, to some extent the fears of liability, because that becomes a very convenient shield in terms of saying “gosh, this is really, really complicated. By the way, we’ve got a burnt-out workforce and we should be challenging them and making it easier for them.”
[00:32:32] Karen Wolk Feinstein: And I know we like to kick the fee-for-service payment system, right? I mean, that is our happiest moment. Hit the pin piñata and everything will improve. But I go to countries that are managed care countries, where there’s no fee-for-service payment. Sometimes they have even worse safety records than we do in the U.S., the business model’s not just about fee-for-service and given what you and Nancy said… I also talked to a CEO of one of our wealthiest systems, and I said to him, “why don’t you care about safety? I mean, it is not on your agenda.” He said, “wake me up when my customers, the employers care. All they wanna do is negotiate on price. No one talks to me about my safety record.” And it may be sad and unappealing, but at least it was an honest response. And I do think that we need to think a lot as customers – people don’t like that – consumers of healthcare, we have to ask for it, how can it be delivered to us magically.
So, one thing that you’ve touched on a number of times, Lisa, Helen, others… data, data, data. We know in aviation, we’re going back now to the late nineties. Um, they created their own protected data system, ASIAS, their aviation safety data system that MITRE actually manages its protective data. But without that real-time, unscrubbed, not recoded data on adverse events and near misses and whatever, the aviation industry could not have done as much as they’ve done to prevent harm before it occurs.
How do we get our industry to come together and somewhat collect safe, protected data that is absolutely accurate?
[00:34:28] Lisa Simpson: Data is clearly one of the key sort of fundamental pieces here, because you need that to target any improvements and monitor progress, obviously. And I wanna also comment that the pandemic has really, I think brought much more focus on our data infrastructure as a country than before. Not just the failings in our public health data systems, but the issue of sharing of data, you know, sharing between states and the federal government. I mean, the CDCs efforts right now with the data modernization initiative. And plans for how they’re collecting data, I think is a good prelude of what it might take or some of the battles ahead for a really enhanced and functional patient safety data system with states really battling some of this. And so, you know, as I think about the data infrastructure, the closest we come really is AHRQ’s Network of Patient Safety Databases and the Patient Safety Organizations. It’s a completely voluntary set of data. And then you’ve got the data CDC collects and this data, I mean, that’s part of the problem, there are all these pockets of data and it’s not coordinated, it’s not uniform.
But I think, you know, if you… going back to that OIG report that you quoted Karen. I mean, they concluded that the PSO program, the patient safety organization program and the, NPSDs, you know, its data had yet to realize its promise. And so we, we have a long way to go. Um, and, um, and yet when you look at the national action plan for patient safety that I mentioned earlier that IHI released. I actually read the whole report again and data… it’s not there. I mean, it’s mentioned in terms of transparency and patient access to the EHRs, et cetera, but an actual national action plan on patient safety data, we don’t have one. And, um, and so I think that’s, that’s an opportunity for Karen, you and others to, you know, figure out how do we get to that in a public-private model of partnership to make that happen.
Now, we’re also talking about workforce burnout. So this data cannot be yet another burden on frontline clinicians. And, you know, we’re a long – we’ve come a long way in the last 30 years on data capabilities. We – I fund and maybe I’m biased, cause I was talking to Karen DeSalvo yesterday at Google and you know about what we can do to get at the data we need that’s not a burden on individual people collecting data and more, um, you know, that sort of additional burden. So I think we need a concerted action plan on the data infrastructure to move forward. Now, maybe you guys are aware of one that I’m not aware of that lays this out. And there’s some really good recommendations in the NAM review of the AHRQ PSO report about that are specific to what data standards and some other issues.
So I hope AHRQ is working on those. So, but I think we need a concerted focus on it. The data’s not gonna magically appear and be comparable and shareable and usable, what, let alone for research. So, what do you think Helen?
[00:37:50] Karen Wolk Feinstein: Well also, let me just say for Carolyn’s comment, we hit – I think Nancy’s been part of the conversation – when we talk about protected data so that people will submit honest data, stop coding it. Everyone who comes from a nursing home who gets a pressure sore, wasn’t present on admission, but until we stop playing these games, it has to be protected. And then the problem is the consumer groups. Go crazy when we talk about, I think you’ve all been part of those conversations, data that’s protected, but I think the most important thing is to make healthcare safer. And if protected data will do that, I’m for it. Helen, I’m sorry, you’re…
[00:38:30] Helen Burstin: Yeah, no, no. I think these are all great points. And actually, I think my response is lots of threads to what people have said. I think back to what Nancy said at the beginning about how I think we had great hope for what Health IT would do. And I think at times it’s made it worse. I think Carolyn’s point about how much we have care is not as much only in the hospital, there’s so much of it now across settings, particularly in the ambulatory care space. And I guess my thought on this is that we have to figure out a way and we just have to, to get to interoperable data. And I think, and I’ve always been a glass half full kind of girl as I think everybody on this call knows – I think we’re at an inflection point. I think these upcoming rules around interoperability and what’s gonna happen with the USCDI, USCDI+, and FHIR, and you can start rattling off all these different standards are going into effect in 18 months.
I mean, unless they get blocked, they’re going into effect. And I think this is a moment, really an inflection point where the patient safety movement that I’ve been encouraging our societies to do this as well… this is your time to say how you want your data to be represented in this new world order of how data’s going to be potentially interoperable. I mean, it, it may not happen in 18 months as planned, but let’s at least put the building blocks in. And I think to Lisa’s point, the idea that your question is about submitting information. I think we’re not gonna get clinicians. Everybody talk that they are completely tapped out. No one’s gonna submit something, but if there’s a way to… through the process of using the data we already have as part of taking care of patients, be able to get some of those key lessons about what happened and really importantly, share it back with clinicians.
We can’t just have this information go out to a PSO if it doesn’t actually come back to the clinicians for learning. I’m always struck by, you know, working with, for example, some of our surgical colleagues who have had these registries. Sometimes the surgeons don’t actually know what happened to the patients at 60 to 90 days, unless it’s part of a registry where they then figure out they got admitted somewhere else. We’ve gotta have that full 360 view of wherever patients went for their care, figure out what that data is, feed it back to the clinicians, feed it back to the hospitals and health systems that Nancy overseas, they’ve gotta have that information that allows them to get that full view of what patient care can be.
So I think we need to build on and take advantage of these emerging regulations that are going into effect… maybe 18 months, maybe two years? But they’re coming. And I don’t think they’re gonna go away this time. And I think it’s time to really think about what the patient safety movement needs and how we get those data in the right format, such that we have apples to apples as we begin comparing each other to our, you know, to each other and really learning. Very much taking this less about a punitive approach and I think it’s really more about how we provide this information back and create a culture of learning and improvement. And I saw there was a question cause I was peeking earlier, but you know a question about financial incentives. I’m not sure this is as much about financial incentives as it is really building on the intrinsic values that clinicians and healthcare workforce bring to the table. Give them the information they need to help take care of patients better.
[00:41:39] Karen Wolk Feinstein: Wow, and you’ve worked on this for a year or two?
[00:41:43] Helen Burstin: Yeah.
[00:41:44] Karen Wolk Feinstein: Don’t give up, keep going, please keep going! I know you’ve built a career here trying to make it happen. So let me, this will answer a number of your questions that I saw in the Q&A. For each of you, what one major change, new requirement, research, policy would be transformative, both to stem the outflow of experienced nurses and doctors and other health professionals, but also to reduce medical errors dramatically. So I’m gonna go in reverse order this time, Lisa!
[00:42:19] Lisa Simpson: Well, Karen, you are always one – if anybody knows you on this call – Karen is bold and fearless. So, you know, I’m gonna try to emulate you just a little bit and I’m gonna suggest something that Washington loves to talk about. And that’s a moonshot. Now, not a moonshot for a dread disease, but what about a moonshot for patient safety? We have to capture the mind and build the momentum. I mean, what if we… I mean, let’s be humble, 500 million to really build the data and learning systems and the workforce we need to get, let’s commit 50, 75% reduction in preventable harm and monitor that. I mean, it’s probably crazy, but hey, let’s shoot for the moon as they say!
[00:43:08] Karen Wolk Feinstein: We have an expression in my religion, “from your lips to God’s ears.” So let me second that Lisa. I’m waiting for the moonshoot. Nancy, how are you gonna get that moonshot? What, what’s your wish?
[00:43:23] Nancy Foster: I don’t know about the moonshot. I’m not as big a thinker as Lisa. I love that idea though. Um, you know, I think we have nuggets of really important advancements. I have the pleasure of being on the Quest for Quality award committee that awards a major accomplishment award on advancing quality to one of our hospitals or health systems every year. This year’s award winner was University Hospitals in Cleveland. And they have done so many of the things that we have preached for low these many years. They’re advancing research. They’re advancing understanding of patient safety. They’re advancing the culture. They have a unique way of involving patients and staff – every member of the staff – it’s this commitment statement where everybody is asked to say, “I will, and then fill in the blank to improve patient safety.” That’s really unique and important.
It’s a way to cement the work within an organization. My one wish is that we could take examples like university hospitals, and really help implement that across the hospital delivery system. It’s, uh, it’s a winning recipe. And everybody on this call, I know knows Dr. Cliff Megerian and Dr. Peter Pronovost who have been responsible for making those advancements at University Hospitals with a whole team of others. That would be my hope.
[00:44:56] Karen Wolk Feinstein: Carolyn, you’re next, thanks.
[00:44:58] Carolyn Clancy: I’m gonna build on first Helen, listening to you a few minutes ago reminded me of how much I miss working with you every day. So, uh, thank you for that – always the glass half full. I wanna build on and foot stomp what Nancy just had to say, but also make another point. First of all, for the past two years, clinicians and patients have had to step forward like never ever before, right. Who knew what it meant to have a loved one at home with COVID, right. The good news is you don’t have to go into the hospital, but you’re really, really sick or you’ve been really, really sick and now we’re letting you go home, but you’re not done for people who really experience the more severe aspects of the disease. I think that we could turn to them and ask, what can we do?
Dr. McWilliams at Harvard, I think has made a very, very compelling series of cases that were under leveraging professionalism among healthcare professionals and I think it’s time to do that. I will also just say that I visited one of our facilities last week. Now this was during a little personal trip for a family event, but it was really amazing. They were having some people present to me on innovations they had done to improve care. Several of these folks were in their first year or transitioned to practice here. You think they’re gonna go work anywhere else? No, because they were encouraged to raise their hands. If you see something to fix or make better, we’re all ears. And I think that we have gotta figure out how to make that real. Now, politically, I think, small P here, we also have to think strategically in terms of some quick wins that we can get right now.
Maybe medication misadventure among the elderly, that’s just a thought for right now, but we could certainly have a reasonable debate. I mean, you have a lot of people on many, many medications and it’s the source of nightmares for me with some of my relatives, friends, and so forth. That might be, you know, something quick and tangible that we could do right now while we are building this culture of commitment and the – I love the “I will” statement – so really appreciate Nancy sharing that. But we’ve gotta be thinking about short, medium, and long-term goals. And that I think will be how we’re gonna get there. Donna Woodson, the chat box has been making the case that we finally have a lot of research that’s starting to bear fruit. But putting some of that in place will take some time and building blocks, but it’s really important to say that we can do X in one year or something along those lines.
[00:47:35] Karen Wolk Feinstein: And I’m going not last, turn to Helen.
[00:47:39] Helen Burstin: So many great suggestions already. So just a yes and. We haven’t talked as much about, I think the power of the patient here. And I think just to harken back to John Eisenberg as were sort of wrapping up a bit here towards the end. He used to always like to say, “patient safety is a team sport and the patient is on the team.” I think we are now in an era that was completely different than John even envisioned it way back when of just where we’re democratizing information about your care. Patients can access their notes. Patients can – again, lots of issues with the digital divide – but patients can look at their lab results. Patients can look at their notes. Patients can reflect back on that. It happens all the time when I precept residents now. So I was like, “Hey, I looked at what you put in the portal. And I have a question.” That’s a change and I feel like if we really wanna build on patient safety, how do we build on ensuring that patients really see a role for themselves in ensuring patient safety and give them some guidance about how to be a really good member of this team to drive it forward.
We’re doing some work a couple of people know with YouTube and Google right now to build on some work the National Academies did last summer looking at criterion principles for what are sources of information, health information for patients on social media. Can we do something like that that helps patients look for and understand, as you’re looking at your information, how can you track and make sure what you’re doing is helping your team as much as possible, be as safe as they can and provide information, reflect on what you’re seeing. And I just, again, I think together we can really be a powerful force for good. I think that this data democratization, as well as the democratization of patients having access to information that used to be only in the realm of clinicians is something we’ve not built enough on. I’m not sure it’s a specific transformative policy, Karen, but I think it’s a movement we should think about how we build on.
[00:49:34] Carolyn Clancy: And Helen, I would just say, we need to consider social media as a data source.
[00:49:39] Helen Burstin: Absolutely.
[00:49:40] Carolyn Clancy: It’s a source of misinformation, but it’s also a source of a lot of information, right, that we don’t routinely mine at all.
[00:49:48] Helen Burstin: Absolutely. Absolutely. I mean, I think if you look – I think it was one of the comments from David at the start of this – I mean I went down the rabbit hole of signing onto TikTok for the first time this weekend as part of this work we’re doing for Google and YouTube… there is a lot of really great information on there. There’s a lot of drack in our, uh, parlance Karen that needs to be cleaned up but at the same time, there’s some really valuable stuff on there. How do we get the safety experts to put out, like all these docs putting out the top five things I wouldn’t do as an OBGYN or the top five things I wouldn’t do in his emergency medicine doc? How can we take advantage of that? There’s millions of people watching those videos.
What are the top five things patients should always look at when a loved one is in the hospital to ensure that they’re safe? What’s the five questions – I remember Carolyn’s initiative when we’re back at AHRQ, you know, questions are the answers. What are the five questions but put it in a way that patients are looking at it – don’t give ’em a handout – make a TikTok, build something in the way that millions of people see it. So again, just that patient engagement piece and you’re right Carolyn the social media aspect of this is just huge right now in ways that our teenage relatives understand in ways that we’re just kind of coming along with slowly.
[00:50:59] Karen Wolk Feinstein: Let me underline that there’s a chapter in a book that just came out by Robert Pearl called, Uncaring, and one of his last chapters are the five questions you should ask your physician. It’s absolutely fantastic. I was thinking this should be out on social media. It should be everywhere. I hate to say it, but I think it could change healthcare. And most people don’t feel empowered to ask those questions, but it is a terrific chapter.
So I’d be remiss and I know someone asked, where are we with the National Patient Safety Board? Moving along, we hope to introduce legislation in September. It would be for an independent, nonpartisan, research and development, organization that would bring multidisciplinary attention to what can we do, particularly, what can we do that would relieve pressure on the frontline and would create safer systems without putting the burden on the people at the front line, not additional burden. So anyway, we’re working on it. We have this amazing coalition. I’ve never been more gratified. 90 organizations representing all the different stakeholder groups have come together. And maybe this time we can bring it over the line. I’m sure hoping that 25 years later that I’ll have something that I can clearly point to other than central line infection, which was the first thank you, AHRQ. Thank you for your support. Without AHRQ and CDC, we would never have delivered on that.
Carolyn, you brought up something really important and that senior care. With all the areas we focused on, we have so much room for improvement in caring for our seniors. I hope that… I look at Singapore as a model – it’s rather extraordinary – but there are others. We can look beyond our borders for some improvements. Maternity care, I go to Australia. But we could be safer and better if we would open our minds. And then the one thing I would say, we had Mark Harrison here speaking at the time, CEO of Intermountain, I think he still is today, but he said something very interesting to the hospitals in attendance. He said, “you aren’t each other’s competition. Your competition is big tech. Your competition is new players in our field because we’re ripe for disruption.”
I would ask all of our legacy institutions, all of you here, people on the call, society associations, agencies, CDC I think has announced that it’s going through a complete reexamination…. could we ask ourselves, we don’t right now need to be disrupted, but what could all of us do and how could our organizations do a really close examination. An industry that isn’t safe is going to be disrupted. It’s gonna be turned upside down. We can’t keep hiding it. And my wish to everyone is every organization look inside. What could you do? How can we make healthcare safer? There are so many good suggestions here. We have so many legacy organizations who have safety in their mission in there and that’s, why they’re on earth. And don’t be disrupted. Get with it. Do whatever CDC’s doing. Reexamine what you’re doing. How do we put safety on speed?
Thank you, AcademyHealth. Thank you so much. It was so wonderful to reconnect with all four of our participants once. Okay, there’s a lot of nostalgia here. We’ve all been at this a long time. All of you have moved through the world of healthcare to bring about so much positive change and may we stay together. May we keep connecting all of us who care a lot about this issue. And may we see real progress because it’s never been tougher what with the aftereffects of a pandemic. So thank everyone for joining in.
If you want a transcript or the show notes with references to related articles and resources, that can be found on our website at npsb.org/podcast/. Up Next for Patient Safety is a production of the National Patient Safety Board coalition in partnership with the Pittsburgh Regional Health Initiative and the Jewish Healthcare Foundation.
It’s executive produced and hosted by me, Karen Wolk Feinstein. Lisa George and Scotland Huber are our associate producers. This podcast was edited and engineered by Jonathan Kersting and the Pittsburgh Technology Council. Special thanks go to Robert Ferguson and Steven Guo. Thank you for listening.
—
